My two cats Ada and Curie having a nice nap together.
Before I got sick I battled with insomnia for many years. It started with living with several extremely noisy housemates at uni that meant what little sleep I did get had to be managed around what quiet time they’d let me have.
Over time this led to such anxiety with getting to sleep that my mind whirred as I tried to rest, so although I’d regularly be exhausted I couldn’t get any rest at all.
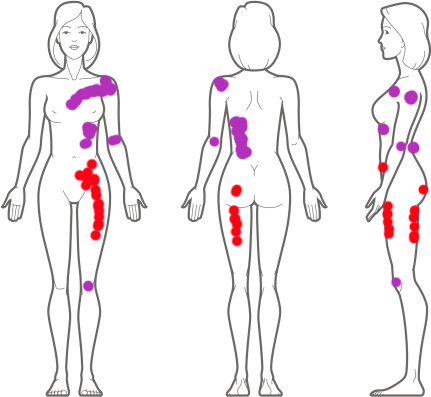
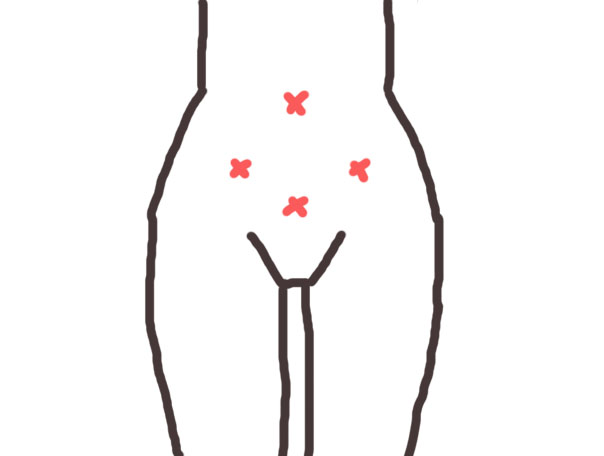
I felt powerless about something that should be effortless, and when I became ill with endometriosis (and started full time work) it was one of the first things I had to sort out to get some quality of life back.
Happily I’ve lived with near perfect sleep since becoming ill, it’s one of the few areas that I don’t have much difficulty with anymore. Although much of my sleep can still be unrestful (and I have wider chronic fatigue problems).
That said, I didn’t quite appreciate how restorative my sleep was until I got a new set of neighbours that caused me several days of restless nights and I got flashbacks to a time that I’d all but forgotten about.
I know some of you must still be in the worst throws of insomnia, and I know how utterly miserable it can be so I’ll do my best to share what has helped me get over that particularly horrible hurdle.
Continue reading →