
Almost ten years after the onset of my first chronic pain condition, I finally got invited to a local NHS run pain management course.
I’ve previously attended the Expert Patient Programme which was also extremely good, however it was not pain/condition specific. I began to feel like I wasn’t given the opportunity to properly assess how well I was managing my pain without a pain management referral.
Other people experiences will vary, but my pain management course was an eight week training session on how to live with pain. It helps you manage flareups, start paced exercise, and help with loads of other things like continuing hobbies and getting a good nights sleep.
Everyone in chronic pain should have the opportunity to learn from experts in pain, and from prior patients, so I’ll explain what pain management is and how to get started.
What is pain management?
This is probably the most important update I have ever written, because in my opinion pain self management is the best way to manage long term-chronic pain.
Pain management teaches you why your pain exists, why it’s not gone away and what you can do to live alongside it rather than fight it.
It does this by teaching you techniques to figure out what you can still do now with pain rather than comparing what you used to be able to do. It helps you create manageable goals to get back your quality of life.
Pain is highly subjective, so there’s no hard and fast rules that will solve your problems, it’s more about learning from the experience of others, getting some advice on what might improve your symptoms, finding the smallest amount you can do without making pain worse (your baseline) and showing you how to increase your activity extremely slowly until you can do more.
Because pain management is so involved, and does require you to make a commitment and maybe even some changes to your current lifestyle, it’s not for everyone but you’ll get out of it what you put in to help yourself.
However how many times have you said you’d do anything to improve your pain, anything at all? Well this is your chance.
Pain management is also quite collaborative, you’re not going to be talked at the whole time, my sessions were quite interactive and you were encouraged to contribute or share your perspective.
What I’ve accomplished because of pain management:
The results speak for themselves, it’s basically about creating good habits and routines, but because of pain self management techniques I have managed to:
- Continue working full time
- Be promoted on three occasions
- To cycle to and from work every day
- To do ~30 minutes of Yoga every day
- Walk for ~40 minutes a day
- Learn another language
- Reduce my medication to the smallest amount it can be
- Sleep better and more easily.
Pain management is the ultimate mechanism for managing with pain and in some places it’s a strangely a well-kept secret. Something that helps you with pain and is free? What’s the catch? (Hard work and perseverance).
Let’s get one thing straight though, it’s not a panacea, it won’t completely rid you of pain, it won’t make you back into who you were, but it will give you your independence back.
I’m telling you this to show you what’s possible. My pain has decreased but I also have more to deal with, and breaking things into an manageable plan completely changed my life and made me better prepared for changes and increased difficulty.
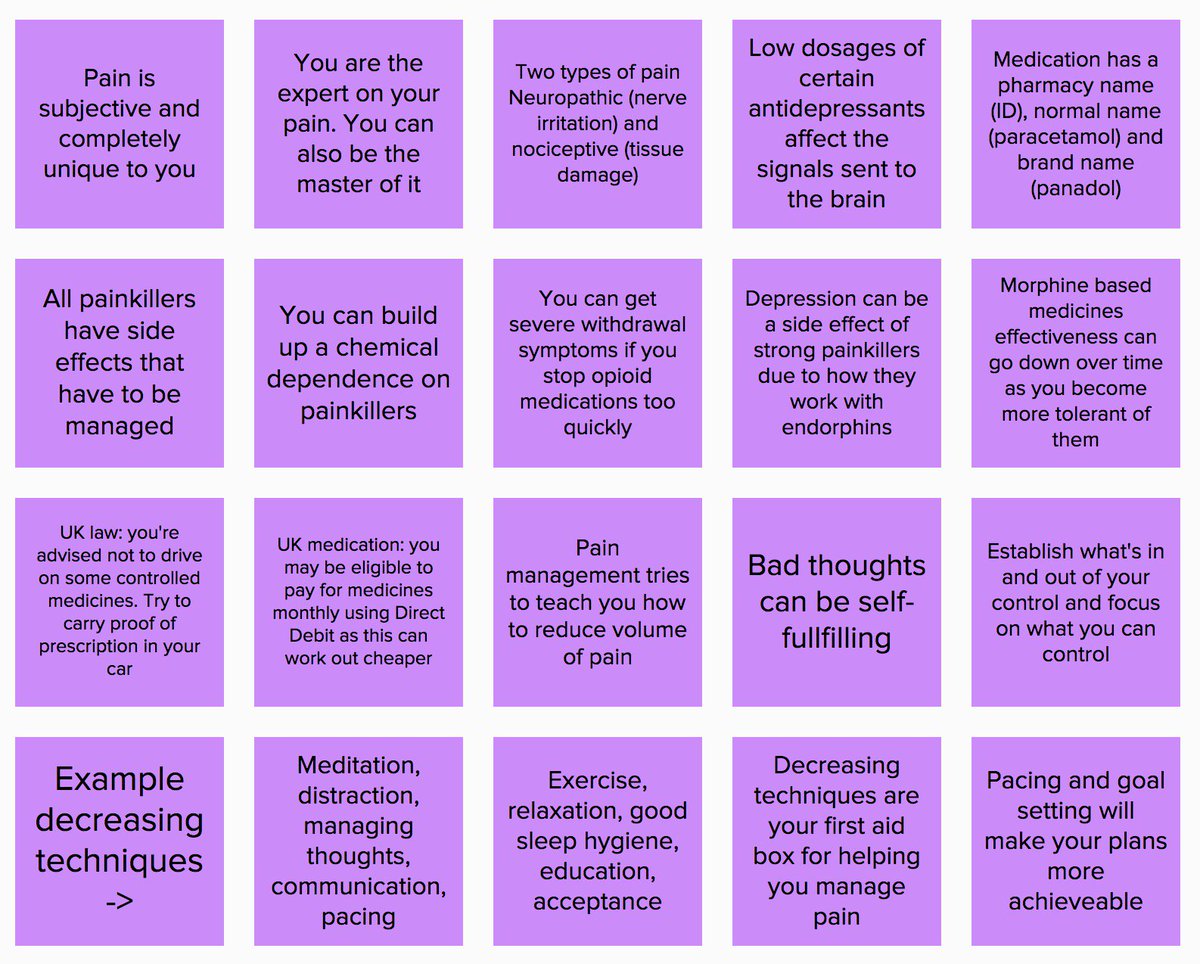
What sort of things do you learn?
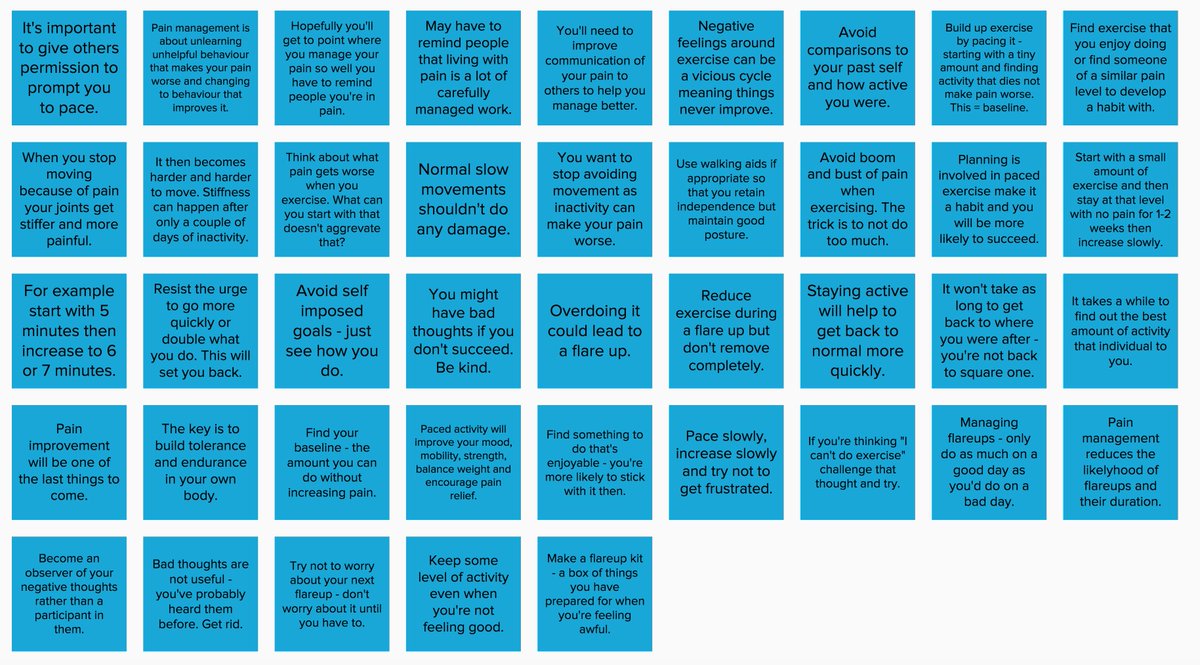
Pacing
Pain management training includes things like learning to pace activities and break them down into smaller pieces with regular breaks. You’ll use this method to get what you want done, it’ll also help you re-evaluate what’s really important, and what you do at the moment that can be stopped or reduced (to make time for you).
You have more to deal with when you live with pain every day. So chronic pain calls for new and inventive ways to live your life when you have more to deal with.
Pain is very individualised so the advice you’ll receive is generic, but they’ll help you to figure out how to apply it for you and your pain circumstances. So this will mean making some improvements and changes in how you live your life. It might seem like you have to do things slowly, but it’s better to do something slowly than do nothing at all.
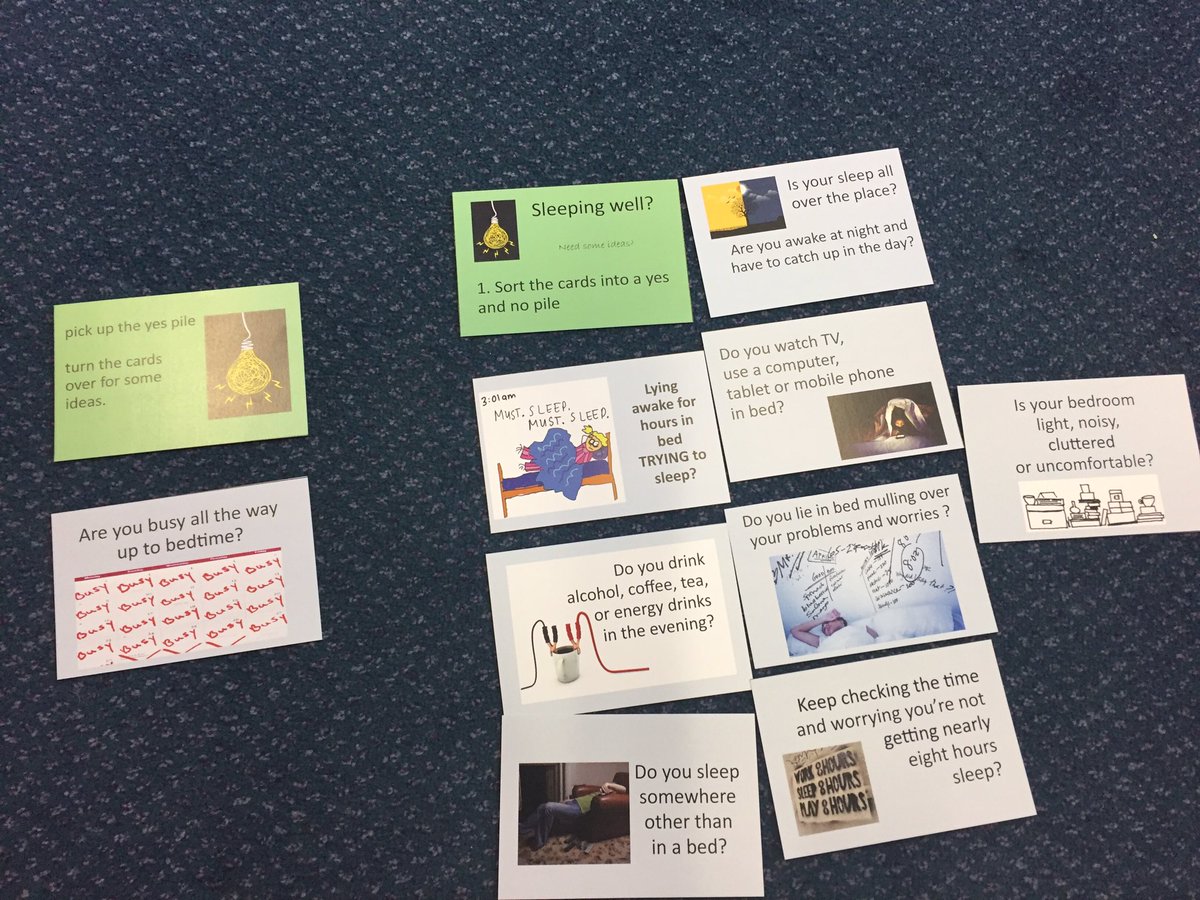
Sleep management
This includes information like how to get a better nights sleep, what might be causing your sleep problems and a long list of ideas of things to try to improve your sleep hygiene. It should also give some ideas of living with and managing fatigue.
Exercise
While this isn’t everyone’s favourite topic exercise remains a key way of managing pain. It’s true that a body that doesn’t move experiences more pain. So pain management will give you some ideas of some low impact activities that will help you get started.
This will include ideas for exercise that start you on something slow and easy and doesn’t make pain worse. This is called finding your baseline – the amount that you can do before pain gets louder. Once you know this you can put together a exercise plan.
In time exercise can become one of the consistent ways to get pain relief, so it’s worth getting a personal plan of how to start from pain management.
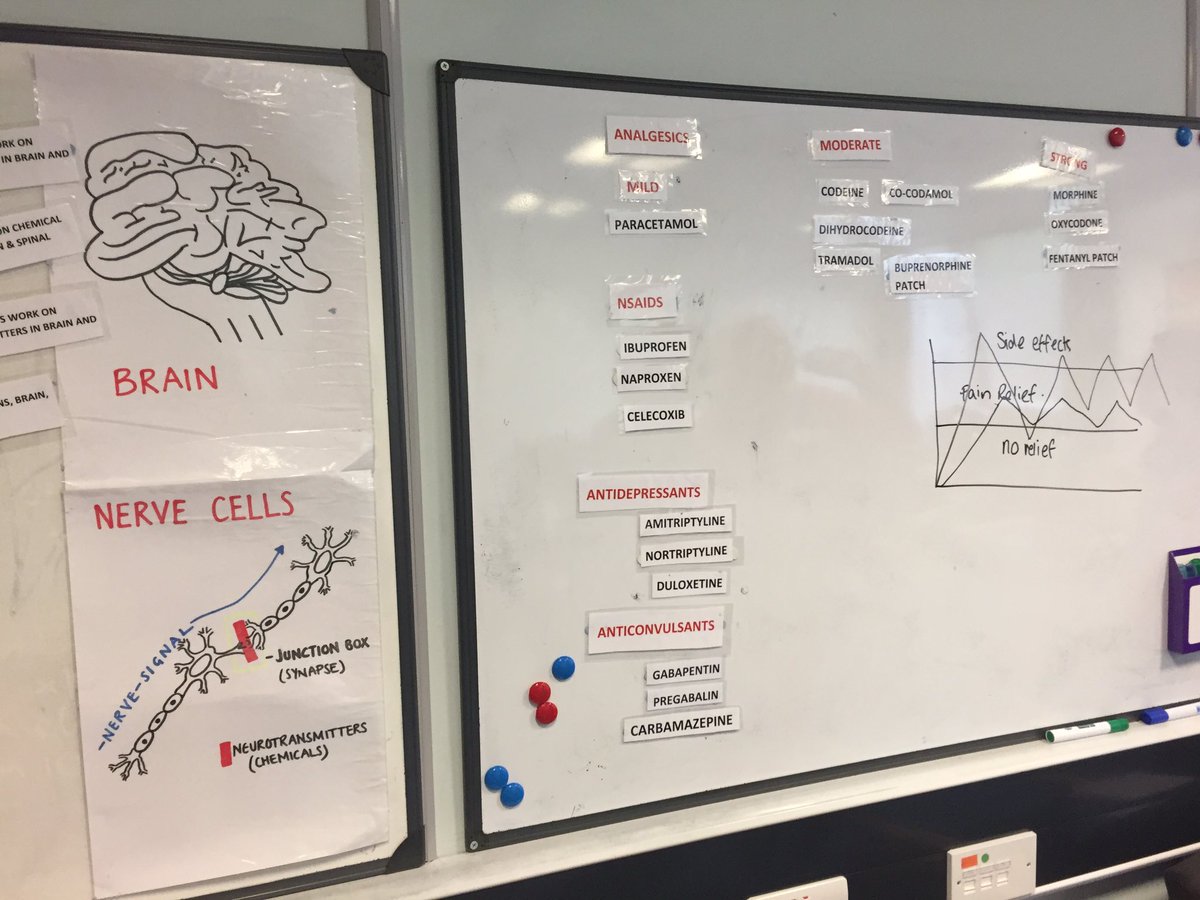
Medication & anatomy
In order to understand how to manage your pain you need to understand how pain works – specifically chronic pain. Being in pain for a long period of time changes how your body interprets pain, and might make you susceptible to things that wouldn’t have bothered you before.
Crucially, you should also find out about your medication. How it works, what side effects it has and how it can operate with other medicines.
Some people like to know the mechanics of how pain works, but if you’re not one of these people this part of the training will remind you of how complicated your body is, and the pain management team may be able to ask your specific questions about pain and side effects and how they interact.
Communication
This is another key part of living with invisible illness. The pain management team will help you to understand how to communicate to others, some conversation tips when things are difficult or people don’t understand. They’ll even explain the different types of communication and how to be assertive in your speech (but not negative). In my course we were asked to bring along someone close to us so they could learn alongside us.
It’s also a good opportunity for another person to explain what living in pain is like. Sometimes the people nearest to you can get used to explanations, but hearing it from someone else can help the ideas sink in.
Managing flareups
Things often don’t go well with chronic pain so learning how to manage flareups is crucial. You’ll be given advice on how to do navigate a flareup, how to reduce the likelihood of one happening, and how to get through one when things seems impossibly hard. The key is to prepare for one before it happens, so you have a flareup plan you can bring into action when things get rough.
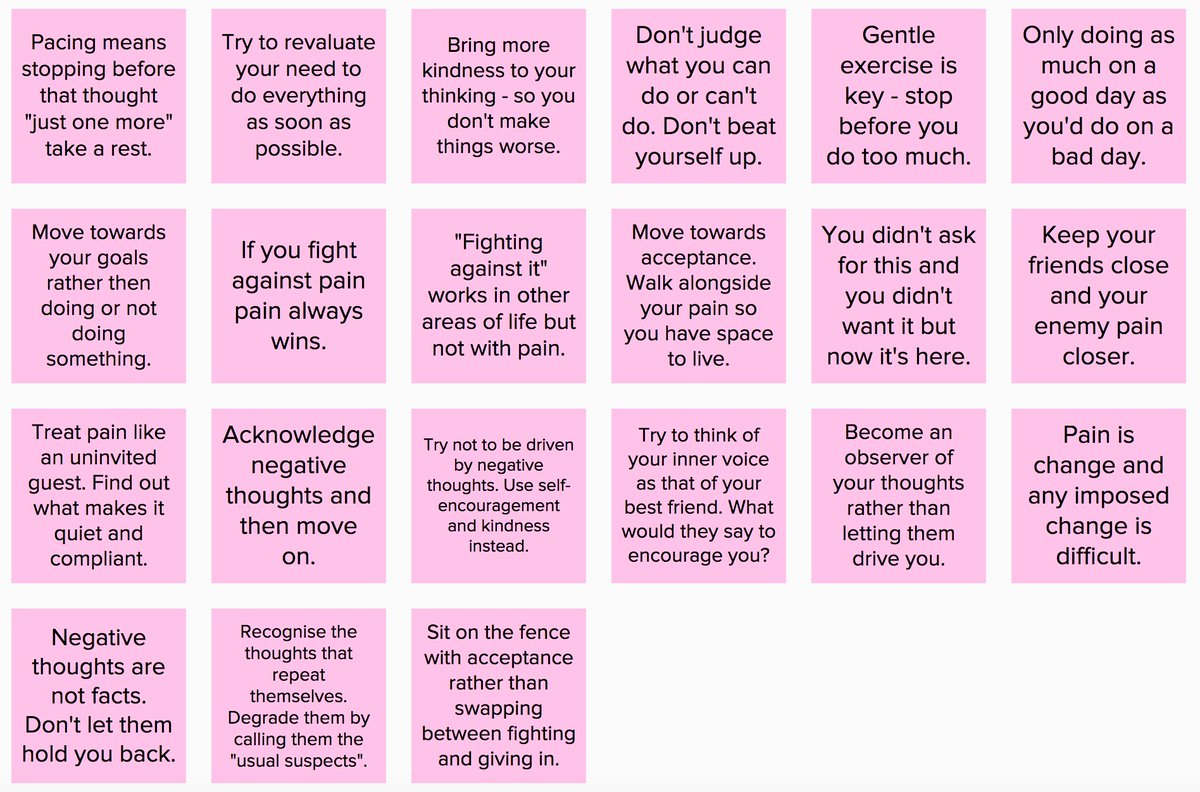
Being kind to yourself
The idea around this is really simple. When living with pain you need to treat yourself like a friend. What would your best friend say to you when you have negative thoughts?
We wouldn’t treat others badly when things are hard so why are we overly unkind to ourselves when the pain is bad? The most useful technique I learnt here was thought capture, the idea of having a negative thought, acknowledging it, but not listening to it, and imagining how your best friend would respond.
Goals and values
You need to have a reason to want your pain to improve. This will be your motivator when things are very hard. Things can get hard while you settle into new routines. Your goals should be achievable and manageable, but broadly it’s your reason to be, your reason to keep going, the things you’re looking forward to.
I can’t tell you what your goal is but pain management may help you to figure it out if it’s not immediately obvious. Goals will be tangible and achievable and it will feel great once you start completing them.
How do I get started?
Most referrals to pain management (in the UK) will require you to be referred to pain management by your doctor or consultant. However you can self refer to a local physiotherapy service and ask them. Physiotherapists may not be aware that they can do this so take along information from your pain management service (either printed or on your phone) to show them they can. Explain your quality of life with pain and ask them for the opportunity to help yourself.
Referrals to pain management are often seen as the option of last resort by GPs or other health professionals so have information prepared to make your case, and keep asking. GPs will usually prefer to give you medication or other treatments but persevere.
You deserve the chance to try and improve your pain levels so please keep pushing to get what you want our of your appointment, and if you can’t manage it on the first occasion, go back and try again, Most doctors will organise it when they realise it’s something you’re not going to let go of.
If you don’t have joy with one doctor, go to another, and another. Keep trying, eventually someone will agree to your request.
Who runs the courses?
It varies, but in the UK courses are generally run by a pain management department in your local NHS. There may be a long waiting list (I had to wait about 3 months for the initial assessment and a future 4 months for the group sessions to start.
So the earlier you get a referral the earlier you can start to get help.
If you wanted to get started on something yourself right now, it might be worth finding finding out if there’s a local Expert Patient session in your area, these are run worldwide and teach pain management techniques for patients by patients. There’s more information on Expert Patients here.
Additionally the pain toolkit will give you practical methodology to get started with. By giving you a numbered set of tools for working through pain, the first of which is…
Acceptance
The first step is to learn to manage your illness, it’s presence and the fact it’s probably not going away. Is to accept that it’s there, and it’s not going away. It’s leaving “why me” or “why can’t I just get better?” thoughts, realising that things putting your life on hold for a period of perfect welcome that may never come.
Pain management is accepting that and saying you’re ready to start working on that wellness now and you’re not waiting for someone else to bring it to you. (Spoiler: someone’s not going to bring it to you).
If you’re there or part of the way there, you’re ready to start helping yourself. And learning how to help yourself is empowering, it’s not about giving up or admitting you can’t do things alone, pain management is all about being taught how to help yourself between appointments, or in connection with your doctor, consultant or medical team, it’s a power-up for you.
Pain management teaches you how to claw back quality of life and gives you tips for finding out what you can still do, because there are still things you can start, return to or continue, you just might need a little help with finding out how.
Good luck, and give me a shout below if you have any questions I haven’t answered.





When a person is in pain, they always need someone who will understand what they’re going through and something to eliminate the pain they’re feeling. Having chronic pain will significantly affect your life including your movement, physical capability, mental and emotional condition. It’s always better to look for non-surgical methods first, depending on the cause of pain. There are different ways to manage it, as advised by Prime Medical Pain Management Center. They believe in a multidisciplinary approach to pain management. From pain medication, physical therapy, chiropractic manipulation, acupuncture, injection to patches, topical ointment and even exercise. Surgery should always be the last resort.
Thanks for this informative post. It is so true that acceptance is really important to move forward rather than fighting the fact you have this disease. I spent too many years fighting it until I started to make some important life decisions that contributed to alleviating my symptoms. I have found one of the best things to help with my pain is exercise, but it needs to be in the form of more gentle exercise like yoga and qigong. I became a fitness instructor as part of my health journey with this disease and I loved it for a time, but I also burned myself out as I was pushing myself too hard which can actually increase inflammation in your body, which is not great for endo! Meditation has been another thing that I cannot live without also, as I find that my pain levels were directly influenced by how stressed or happy I felt. The happier I could get within myself (which is obviously a challenge when you are dealing with pain) the better my symptoms became. I write like this is all in the past, because it mostly is now-I feel as if I have beaten stage four endometriosis through variety of lifestyle changes, and mostly mental and emotional changes. I am rarely in pain now and I feel it is a result of an 8 year journey I took to help myself.
Well done on stepping up and being determined to get on with your life no matter what. The information you are delivering here is really important for others in the throws of suffering endometriosis-especially if they have been newly diagnosed and not sure which way to turn.
Thanks for helping me learn more about pain management. I actually didn’t know that one of the things that is involved with this is learning how to pace different activities. I can definitely see the benefits of this, especially if you need something specific for your situation. I’m curious to learn what some general tips are for certain pain, or maybe even some other methods that people have done. Perhaps their advice could be useful.
It’s worth giving pain management a try, it’s one of the best things I’ve ever done for my pain. It’s hard work though and therefore often overlooked.
Very informative post…All the given points will definitely help the people who has gone through such situation.